[ad_1]
Between 2019 and 2023, antibiotic consumption in the EU increased by 1%, moving further away from the 2030 target of a 20% reduction recommended by the Council of the European Union.
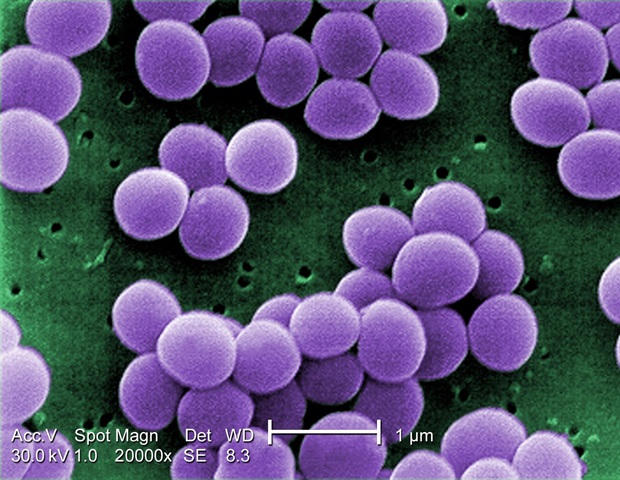
Although there have been significant reductions in methicillin-resistant Staphylococcus aureus bloodstream infections during the same period, the situation in other critical areas, such as carbapenem-resistant Klebsiella pneumoniae bloodstream infections, has worsened, with an increase in incidence by almost 60% between 2019 and 2023. This represents a growing threat to patients in hospitals across the EU, particularly since very few therapeutic options remain available to treat patients infected with carbapenem-resistant K. pneumoniae.
Reaching the EU targets by 2030 requires a united, urgent response across the EU to prevent AMR from undermining healthcare. This response is key to protecting patients and sustaining the effectiveness of antibiotics for future generations.”
Dr. Pamela Rendi-Wagner, ECDC Director
To highlight the serious threat presented by antimicrobial resistance (AMR), ECDC has launched a series of patient stories to give a voice to people who have experienced prolonged hospital stays, uncertain recovery and complex treatments due to AMR. The stories also talk about the impact that these infections have had on the patients’ lives and families.
While some Member States have made great progress towards their recommended AMR targets, or even in some instances have already reached the recommended targets, the overall picture shows that more specific, intensified interventions are urgently needed across the EU.
To turn the tide in the fight against AMR, ECDC is calling for accelerated efforts in three main areas: infection prevention and control, prudent use of antimicrobials, and the development of and access to novel antimicrobials.
Healthcare-associated infections account for 70% of the AMR-related health burden in the EU. This is why hospitals must prioritise basic, yet critical measures for infection prevention and control, such as:
• improving hand hygiene and giving easy access to alcohol-based solutions for hand disinfection,
• increasing screening for the carriage of resistant bacteria to curb the growing trend in carbapenem-resistant Klebsiella pneumoniae,
• increasing the capacity to isolate positive patients by making sure that there are enough single rooms,
• increasing the number of dedicated infection prevention and control staff and relevant training.
The community sector accounts for 90% of total antibiotic use in humans. Reducing the use of antibiotics requires more information and public awareness campaigns, complemented by social and behavioural interventions to prevent their unnecessary use.
ECDC continues to promote the development of and access to novel antimicrobials, and alternatives to antimicrobials, that are both effective and safe for humans. Antimicrobials of this type are essential for treating patients with infections that are resistant to last-line antibiotics such as carbapenems.
In the absence of stronger and swifter public health action, it is unlikely that the EU will reach all its targets by 2030. The consequence will be an increased number of infections with antimicrobial-resistant bacteria that will be more difficult to treat, leading to increasing challenges for patients and larger numbers of AMR-related deaths.
ECDC is committed to supporting Member States in achieving their 2030 AMR targets and has a range of measures to help them address specific gaps and strengthen national capabilities. These include individual AMR country visits and regular Public Health Emergency Preparedness Assessments for all EU/EEA countries, with antimicrobial resistance and healthcare-associated infections as key focus areas.
[ad_2]
Source link